By Jo Ann Kauffman, MPH
President/Founder, Kauffman and Associates, Inc.
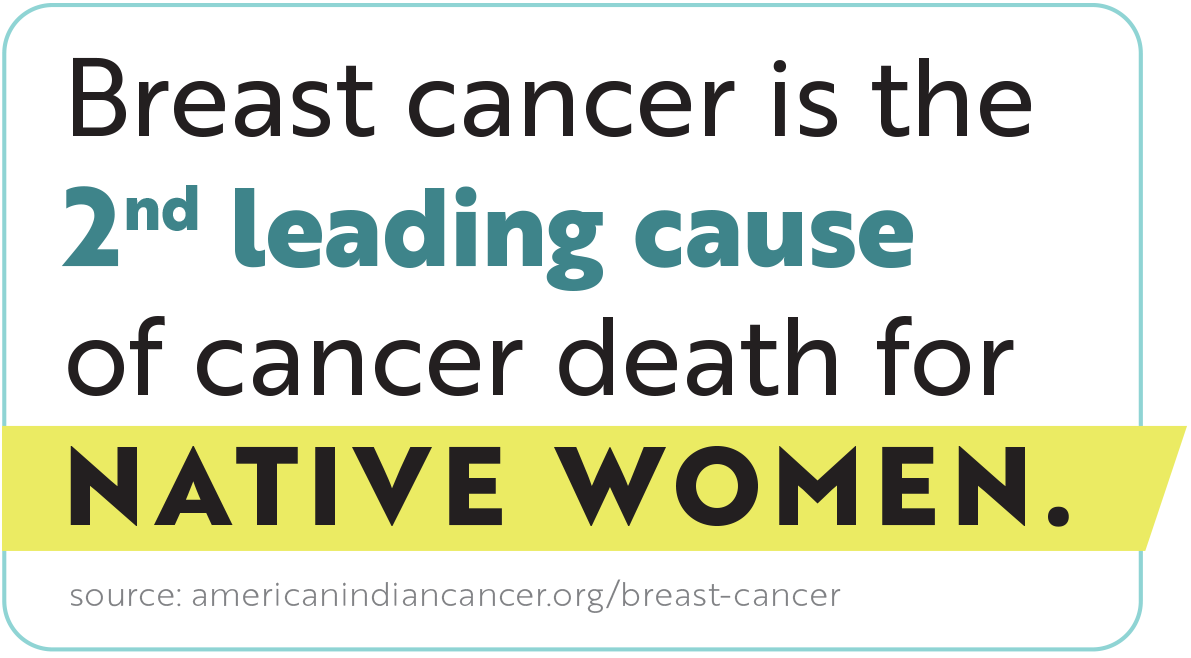
In 2020, while the rest of the country was in the throes of COVID-19, I was diagnosed with breast cancer. Not just any breast cancer…. Stage 3, metastatic Triple Negative Breast Cancer (TNBC) to be exact. An aggressive little beast. This came as quite a shock. I was trained in public health and had been obsessively disciplined about getting mammograms every year since turning 35, even paying the extra bucks for new fancy 3-D mammograms when they became available. In fact, I had gotten a 3-D mammogram only 9 months before my diagnosis. What went wrong?

There were a couple of risk factors working against me that I should have taken more seriously. First, over the decades of getting mammograms I always noticed the small print at the bottom of each mammogram report. It said in essence, ‘you have dense breasts and mammograms might not be reliable screens for women with dense breasts’ (paraphrasing). It means that the breast tissue is more fibrous with more milk-producing tissue than fat, making cancers more difficult to detect on a mammogram. I dismissed this fine-print and embraced dense breasts as a badge of honor. “Yes, I am a proud, strong Native woman with hella dense breasts!” Unfortunately, even today routine breast screening technology may not work for women with dense breasts, despite the fact that half of all women over 40 have dense breasts. Talk about dense!
In 2023, the Food and Drug Administration (FDA) finally changed its regulations over mammograms to require providers to better inform women with dense breasts about the limits of mammogram findings and help them find ways to improve screening. While this new FDA rule continues to place the burden on the woman to seek out more resources, it does require providers to do more than just provide a footnote on the report. It will also help with insurance coverage for covering costs for better screening, such as asking for (demanding) an ultrasound or MRI.
If your mammograms include a notation that you have ‘dense breasts’, please please please, don’t ask, but DEMAND additional screening, such as an ultrasound or MRI.
My second factor was a genetic risk. This is a tough one, as you don’t know until you know. Three of my five sisters and several first cousins on the father’s side had already been diagnosed with and overcome various forms of breast and other cancers before my diagnosis. Getting a genetic test paid by insurance can be a challenge, but it’s worth the investigation. Your primary provider can push your insurance carrier if you can make the case there is a family history. Mapping cancers across the generations and across your extended family is an important first step. If there are trends or multiple cancers, ask for genetic testing. Once you know your genetic risk, you can take preventative actions to reduce that risk, such as more aggressive screenings and/or preventive surgeries. If you carry a genetic risk, there is a 50/50 chance this gene might be passed to a child. Adult children should know their risk, so they can make their own decisions about testing and screening.
I decided to have a double mastectomy, even though only one breast was affected by the cancer. The genetic risk for recurrence in the other breast was much too high. In fact, genetic risks can be so substantial that double mastectomy is an option even if there is no cancer, as a prophylactic measure.
I am happy to report that after an intense year of aggressive treatments, four surgeries, followed by four years of screenings, I am cancer free today. Woo Hoo!!
I continue to screen to make sure it stays that way.

It has been a long battle that I survived only through the love and support of my children, grandchildren, sisters and extended family, friends, prayer-warriors, excellent medical providers, and of course the constant presence of a loving Creator. It taught me the power of presence and peace. It taught me to treasure the laughter and/or the tears of right now, and grace to accept the helpers and healers who bring their medicines into my home to share prayers, songs, traditional foods, and healing.
My youngest, Julia, relocated from NYC to Spokane to live with me during the chemo, radiation, and surgical treatments. We lived together that first year. We were COVID Bubble Buddies. Yep, 2020 was my year of the 3Cs (Covid, Cancer, Chemo). My only demand for her and for all my children was to make me laugh at least once a day, and they did! When my brain was too fried to read, they got me into audiobooks and gave me a Jason Mamoa coloring book. I went sledding, rode a scooter, and adopted a 3-legged dog. At one point I was mistaken for a little boy while waiting in line at a cannabis shop. I looked like a kid, standing there in baggy jeans, a baseball cap, with a flat chest. “Hey, you have to be 21 to be in here!”, the man barked. “I am a 68-year-old grandma!” I replied. We had some good tearful laughs.

Early on, a good friend Barbara Aragon (also a breast cancer survivor) said to me, “It’s like ceremony. You will go through your treatments like ceremony”. She was so right! Similar to Anne Lamott’s ‘Three Essential Prayers’, every day began as a prayer of gratitude for just being alive, (thank you!) and for the strength and peace to move through whatever that day would require (help me) … But mostly just absorbing the amazement of the beautiful people and sights along the way: fantastic sunsets, blue sky with no jet-stream in sight, glistening white snow perfect for my sled, deep tearful conversations, a knowing smile from a stranger, an unexpected visit from a longtime friend, a spontaneous extended family zoom meeting led by our younger generation singing and praying.. and that beautiful old cancer patient who, upon completing the final session of his chemo treatments, shuffled slowly past the 15-20 of us tethered to chemo drips at the cancer care center giving us each a nod and thumbs up saying, “you gonna be fine.. you’ll get through it”…(wow!).
After receiving a TikTok message from my 12-year-old grandson, Patrick, (who was only 7 during my cancer treatments) expressing his relief that I survived, I realized this wasn’t just my journey, but his and others’ as well. I wanted to share my cancer story in hopes it will motivate you (the reader) to self-advocate for better screenings in addition to mammograms, especially if you have dense breasts. You deserve the BEST screening and the BEST care! Inquire about your genetic or other risk factors. Get ahead of your health care. Be your own advocate for the best screenings and advanced tests for your unique situation. You deserve the best.
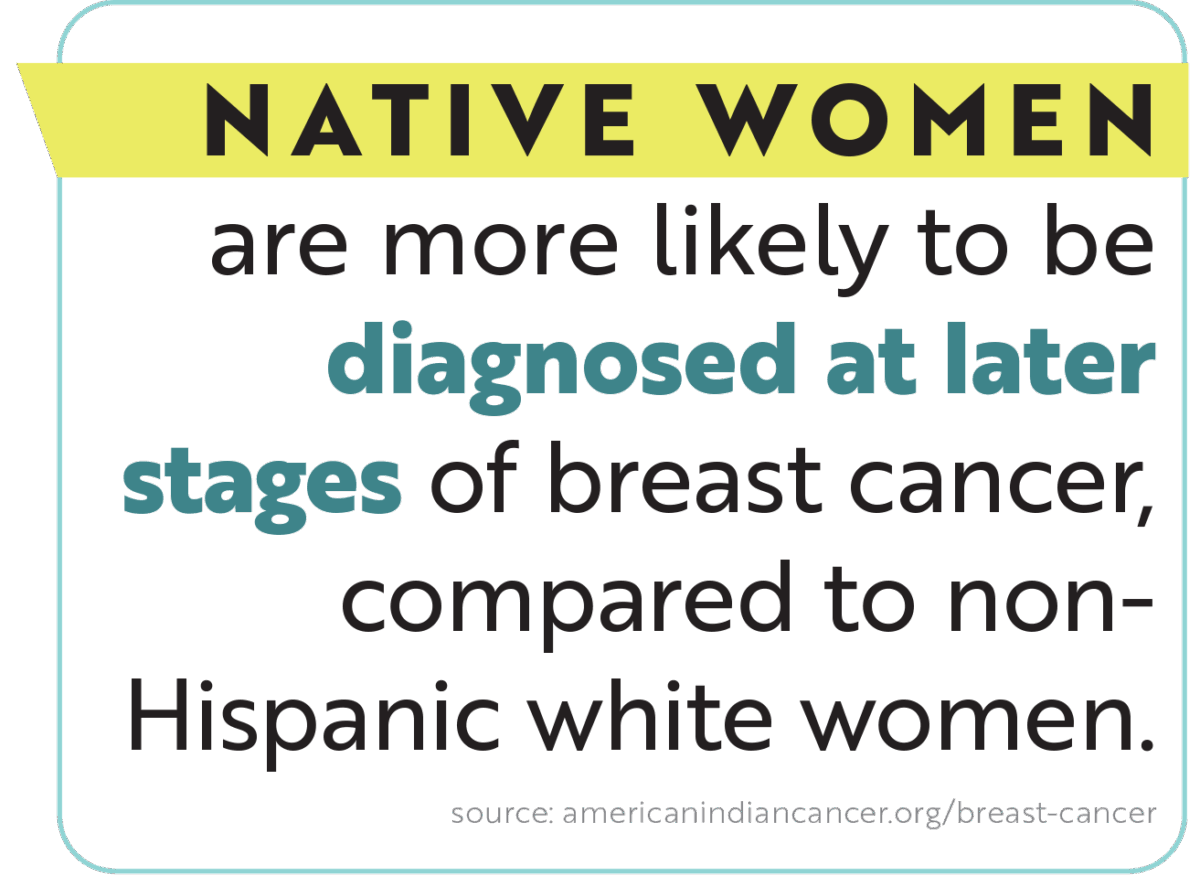
Know your risks. Examine breasts regularly and report any lump or abnormality immediately to your health provider. Get regular mammograms. If you have dense breasts, ask for MRI or ultrasound screens. Don’t wait.
No matter the twists and turns of your journey, find your voice, seek the best care, find joy, peace, and community along the way, no matter what. You are sacred. It is ceremony.
For more information:
https://americanindiancancer.org
https://www.uihi.org/health-initiative/urban-cancer-solutions-by-american-indian-cancer-foundation/
https://www.fightlikeagirlfoundation.org/
https://www.komen.org/about-komen/our-impact/breast-cancer/breast-cancer-awareness-month/